Antimicrobial Resistance and Hypervirulent Klebsiella pneumoniae: Global Situation
Hypervirulent Klebsiella pneumoniae poses a critical global threat in 2024, with rising antimicrobial resistance and limited treatment options.
1. Introduction
Antimicrobial Resistance, Hypervirulent Klebsiella pneumoniae is a significant cause of healthcare-associated infections worldwide. The rise of hypervirulent strains and the increasing prevalence of antimicrobial resistance (AMR) pose a serious public health threat. Hypervirulent Klebsiella pneumoniae (hvKp) is particularly concerning due to its enhanced virulence, leading to severe infections even in healthy individuals.
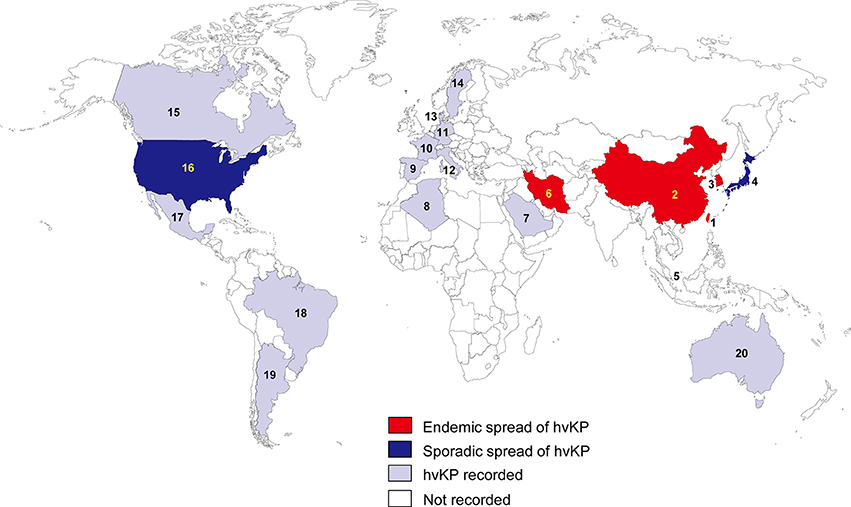
2. Global Epidemiology
The global spread of hypervirulent and multidrug-resistant (MDR) Klebsiella pneumoniae strains has been documented in various regions, including Asia, Europe, and the Americas. The combination of hypervirulence and AMR complicates treatment and increases mortality rates.
- Asia: Particularly in China and Southeast Asia, hvKp is prevalent. It is often associated with liver abscesses, meningitis, and other invasive infections.
- Europe: Several outbreaks of MDR hvKp have been reported, especially in healthcare settings.
- Americas: The United States and Latin American countries have reported increasing cases of hvKp, often linked to healthcare-associated infections.
3. Antimicrobial Resistance Mechanisms
Klebsiella pneumoniae has acquired various resistance mechanisms, including:
- Extended-spectrum β-lactamases (ESBLs): These enzymes confer resistance to cephalosporins and monobactams.
- Carbapenemases: Resistance to carbapenems, often considered last-resort antibiotics, is particularly concerning. The most common carbapenemases in K. pneumoniae include KPC (Klebsiella pneumoniae carbapenemase), NDM (New Delhi metallo-β-lactamase), and OXA-48-like enzymes.
- Colistin Resistance: The emergence of colistin resistance, often mediated by the mcr-1 gene, is alarming since colistin is used to treat MDR infections.
4. Challenges in Diagnosis and Treatment
The dual threat of hypervirulence and antimicrobial resistance makes diagnosis and treatment challenging. Standard laboratory tests may not identify hvKp, and treatment options are limited due to resistance. Combination therapy and novel antimicrobials are being explored as potential solutions.
5. Public Health Implications
The global spread of hvKp poses a significant threat to public health. The high transmissibility and virulence of these strains, coupled with limited treatment options, could lead to increased mortality and healthcare costs. Surveillance, infection control measures, and research into new treatment options are critical to addressing this threat.
6. Future Directions
- Surveillance: Enhanced global surveillance to monitor the spread of hvKp and AMR.
- Research: Development of new antimicrobials and vaccines targeting hvKp.
- Infection Control: Implementation of stringent infection control practices in healthcare settings.
References
- Shon, A. S., et al. (2013). Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: A new and dangerous breed. Virulence, 4(2), 107-118.
- Paczosa, M. K., & Mecsas, J. (2016). Klebsiella pneumoniae: Going on the offense with a strong defense. Microbiology and Molecular Biology Reviews, 80(3), 629-661.
- Wyres, K. L., & Holt, K. E. (2018). Klebsiella pneumoniae as a key trafficker of drug resistance genes in the human microbiome. Nature Reviews Microbiology, 16(6), 315-330.
- Russo, T. A., & Marr, C. M. (2019). Hypervirulent Klebsiella pneumoniae. Clinical Microbiology Reviews, 32(3), e00001-19.